Alzheimer’s disease early onset hesi case study is a comprehensive examination of the clinical presentation, diagnosis, and management of Alzheimer’s disease (AD) in younger individuals. This study provides valuable insights into the unique challenges and complexities associated with AD in this population.
This case study explores the clinical manifestations, diagnostic criteria, differential diagnosis, pathophysiology, biomarkers, and treatment strategies for early-onset AD. It also discusses the nursing considerations, research efforts, and future directions in the field.
Overview of Alzheimer’s Disease Early Onset: Alzheimer’s Disease Early Onset Hesi Case Study
Alzheimer’s disease early onset (EOAD) is a neurodegenerative disorder characterized by progressive cognitive and functional decline in individuals under the age of 65. It accounts for approximately 5-10% of all Alzheimer’s cases. EOAD is associated with a higher genetic risk compared to late-onset Alzheimer’s, with mutations in genes such as APP, PSEN1, and PSEN2 being common.
Environmental factors, such as head trauma, smoking, and air pollution, may also contribute to its development.
Clinical Manifestations and Diagnosis
The clinical manifestations of EOAD are similar to those of late-onset Alzheimer’s, including memory loss, difficulty with language, and impaired executive function. However, the progression of symptoms tends to be more rapid in EOAD. The diagnosis of EOAD involves a comprehensive assessment, including a detailed medical history, physical examination, and cognitive testing.
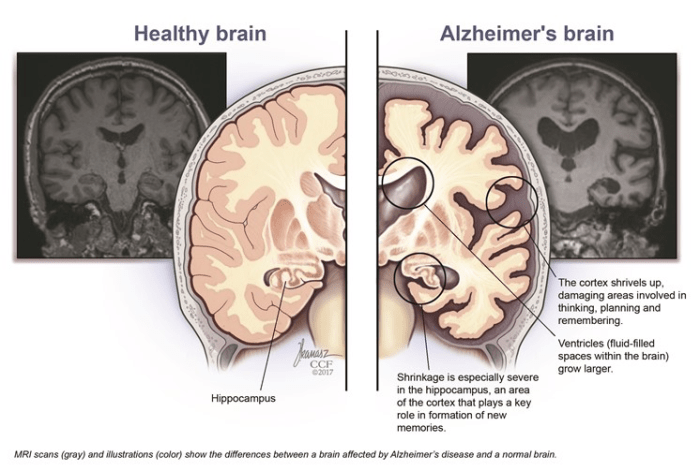
Neuroimaging techniques, such as magnetic resonance imaging (MRI) and positron emission tomography (PET), may be used to support the diagnosis.
Differential Diagnosis and Comorbidities, Alzheimer’s disease early onset hesi case study
The differential diagnosis of EOAD includes other conditions that can cause cognitive impairment in younger individuals, such as frontotemporal dementia, Lewy body dementia, and vascular dementia. Comorbidities commonly associated with EOAD include depression, anxiety, and cardiovascular disease. These comorbidities can impact the progression of Alzheimer’s and affect the overall quality of life.
Pathophysiology and Biomarkers
The underlying pathophysiology of EOAD involves the accumulation of amyloid plaques and tau tangles in the brain. Amyloid plaques are composed of a protein called amyloid-beta, while tau tangles are composed of a protein called tau. These pathological changes lead to neuronal dysfunction and loss, resulting in the characteristic cognitive and functional decline.
Biomarkers, such as amyloid-beta and tau proteins, can be measured in cerebrospinal fluid or blood to aid in the diagnosis and monitoring of EOAD.
Management and Treatment Strategies
The management of EOAD involves a combination of pharmacological and non-pharmacological interventions. Pharmacological treatments include cholinesterase inhibitors and memantine, which aim to improve cognitive function. Non-pharmacological interventions include cognitive stimulation therapy, physical activity, and social engagement, which aim to maintain cognitive function and quality of life.
Question & Answer Hub
What are the risk factors for early-onset Alzheimer’s disease?
Risk factors for early-onset AD include a family history of AD, certain genetic mutations, head injuries, and vascular risk factors such as hypertension and diabetes.
What are the common symptoms of early-onset Alzheimer’s disease?
Common symptoms include memory loss, difficulty with language, impaired judgment, and changes in behavior and personality.
How is early-onset Alzheimer’s disease diagnosed?
Diagnosis involves a comprehensive evaluation including a medical history, physical examination, cognitive assessment, and brain imaging.
What are the treatment options for early-onset Alzheimer’s disease?
Treatment options include medications to manage symptoms, lifestyle modifications to promote brain health, and supportive care to address the challenges of living with AD.